Medical credentialing is crucial in optimizing Revenue Cycle Management (RCM) for small medical practices. Here’s how effective credentialing can enhance RCM processes:
1. Ensuring Compliance and Reducing Denials
Credentialing ensures that healthcare providers are properly verified and meet the necessary qualifications and standards. This reduces the risk of claim denials due to provider credentialing issues, thus streamlining the billing process and improving cash flow.
2. Enhancing Contract Negotiations
With proper credentialing, practices are better positioned to negotiate favorable terms with insurance companies. Credentialed providers often have access to higher reimbursement rates and better contract terms, which positively impacts revenue.
3. Speeding Up the Claims Process
Credentialed providers are more likely to have their claims processed promptly by insurers. This expedites the reimbursement process and reduces delays associated with unverified or improperly credentialed providers.
4. Improving Provider-Payer Relationships
Credentialing helps build trust with payers by demonstrating that a practice adheres to industry standards and regulations. This can lead to smoother interactions and fewer disputes, contributing to a more efficient RCM in medical billing.
5. Facilitating Accurate Billing
Credentialing ensures that provider information is up-to-date and accurate. This accuracy is crucial for correct billing and coding, reducing errors that can lead to rejected claims and financial losses.
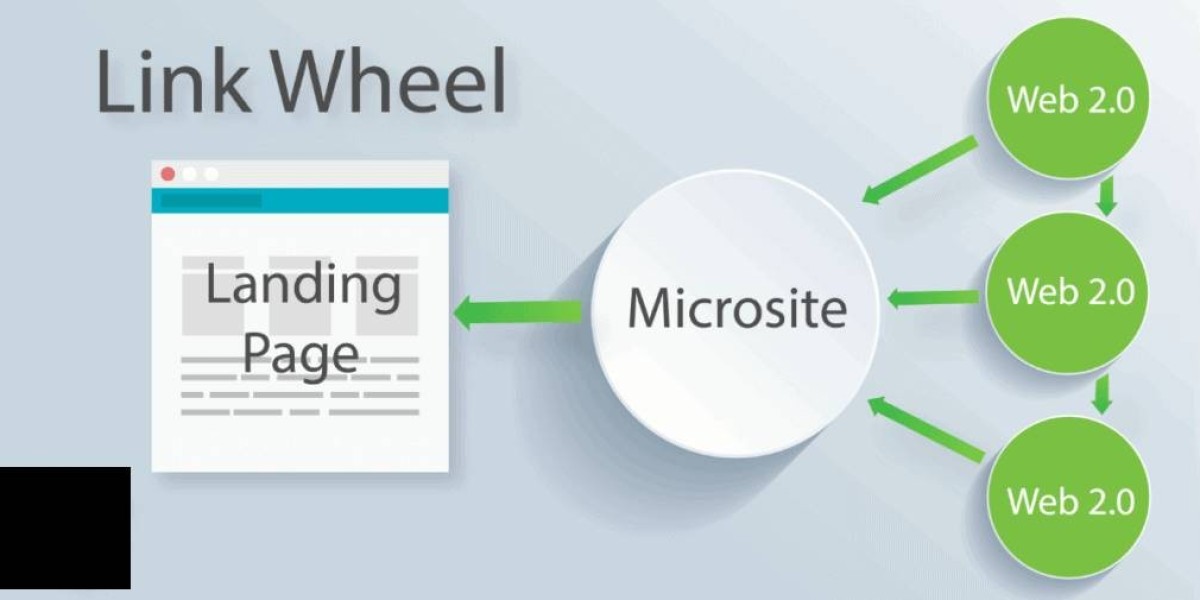
6. Streamlining the Enrollment Process
Proper credentialing simplifies the provider enrollment process with insurance companies. Once credentialed, providers can more easily join new insurance networks, expanding their patient base and potential revenue.
7. Enhancing Patient Trust and Satisfaction
When providers are properly credentialed, patients are assured of receiving care from qualified professionals. This can enhance patient satisfaction and lead to higher patient retention rates, indirectly benefiting the practice’s revenue cycle.
8. Reducing Administrative Burdens
Effective credentialing processes reduce the administrative burden on practice staff by minimizing the need for follow-ups and corrections related to credentialing issues. This allows staff to focus more on optimizing other aspects of RCM.
9. Supporting Accurate Data Reporting
Credentialing helps ensure that the data submitted to payers is accurate and up-to-date. Accurate data reporting is essential for receiving proper reimbursements and maintaining financial health.
10. Facilitating Compliance with Regulations
Credentialing ensures that practices comply with regulatory requirements and industry standards, helping to avoid penalties and fines that can affect the financial stability of small practices.
In summary, medical credentialing is a foundational element that supports the optimization of medical billing services for small practices. By ensuring compliance, improving accuracy, and facilitating better relationships with payers, credentialing helps small practices streamline their revenue cycle and enhance overall financial performance.