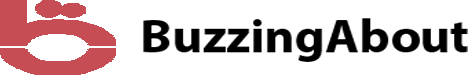
When seeking treatment for drug or alcohol addiction, understanding your insurance coverage can make the process less stressful. UMR, a third-party administrator affiliated with UnitedHealthcare, offers coverage that may include drug and alcohol rehabilitation. For those in Arizona, knowing the details of UMR rehab coverage can be crucial in choosing the right treatment program while managing costs effectively.
What Is UMR Insurance?
UMR is a health insurance plan administrator, offering customized benefits packages for employers. It works as a liaison between health providers and employees, managing claims, benefits, and coverage options. UMR is known for its flexible plans that aim to cater to the unique needs of individuals, including drug and alcohol rehabilitation.
Because UMR works with UnitedHealthcare, policyholders often have access to a wide range of in-network providers. This can make finding a rehabilitation facility easier and more affordable for individuals who need treatment in Arizona.
Does UMR Cover Drug and Alcohol Rehab?
Yes, UMR typically offers coverage for drug and alcohol rehabilitation as part of its mental health and substance use disorder benefits. The level of coverage can vary depending on the specific plan an individual holds. Rehabilitation services that are often covered under UMR plans include:
Inpatient Rehab: This involves staying at a rehabilitation facility for intensive, structured care. UMR rehab coverage usually includes a percentage of the cost of inpatient stays, but the specifics depend on your plan.
Outpatient Rehab: For those who prefer to stay at home while receiving treatment, outpatient rehab offers flexibility. UMR plans often cover counseling and therapy sessions, as well as medical evaluations.
Detox Programs: Before beginning rehabilitation, some individuals may need to undergo detoxification to safely remove substances from their system. UMR may cover medically supervised detox programs as part of its substance use disorder treatment options.
How to Verify UMR Rehab Coverage in Arizona
To confirm your coverage, it’s essential to verify your benefits directly with UMR. Here are steps you can take to ensure you understand what’s included in your plan:
Contact UMR Customer Service: By reaching out to UMR’s customer service or your plan administrator, you can clarify what portion of drug and alcohol rehab costs will be covered. They can provide detailed information about in-network and out-of-network facilities in Arizona.
Check Your Policy: Each UMR plan can differ significantly, so reviewing your policy’s fine print will help you understand deductibles, co-pays, and other costs. Pay special attention to the specific rehabilitation benefits included.
Pre-Authorization: In some cases, UMR requires pre-authorization before you enter rehab. It’s crucial to get this approval to ensure that your coverage applies when you start treatment.
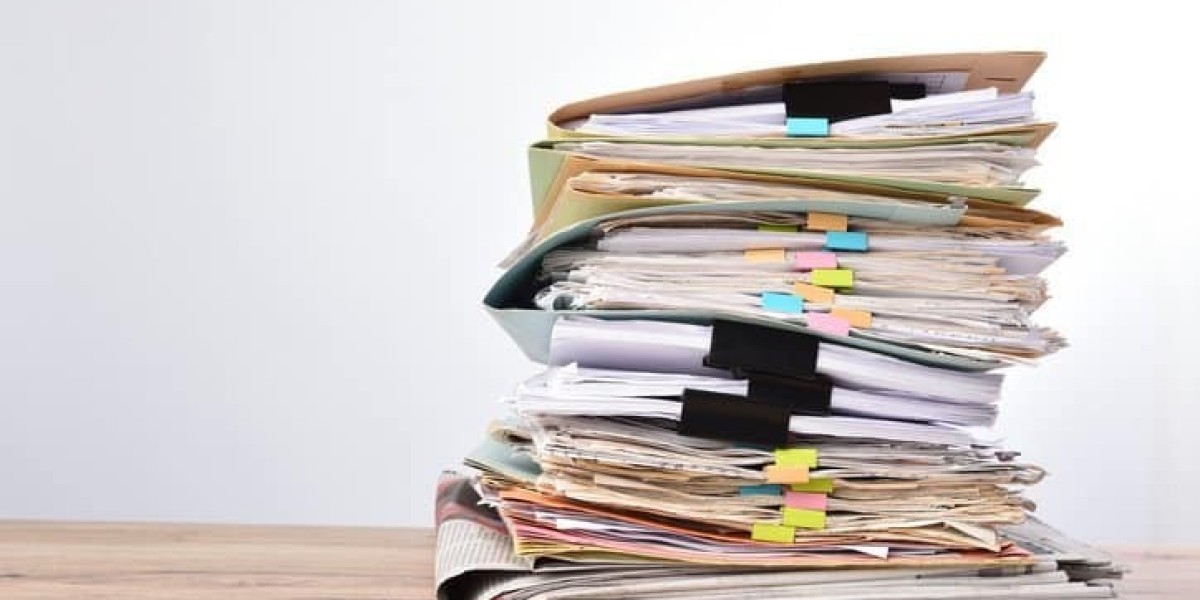
In-Network vs. Out-of-Network Rehab Centers
When seeking rehab in Arizona, choosing an in-network facility can significantly reduce your out-of-pocket costs. UMR has contracts with a variety of drug and alcohol rehabilitation centers across the state. By staying within the network, you may benefit from lower deductibles, co-pays, and higher reimbursement rates.
If you opt for an out-of-network facility, UMR rehab coverage may still apply, but you will likely pay a larger share of the costs. Verifying whether the facility you are considering is in-network can prevent unexpected expenses.
Arizona Drug and Alcohol Rehab Services Covered by UMR
Arizona is home to a variety of treatment centers offering comprehensive care for addiction recovery. The types of services that UMR often covers in Arizona include:
Residential Treatment Programs: These are long-term inpatient programs that provide 24-hour care and are usually best for individuals with severe addictions. UMR may cover part of the cost depending on the length of stay and treatment needs.
Partial Hospitalization Programs (PHP): These programs provide structured treatment during the day but allow patients to return home at night. PHPs are a flexible option for those who need more care than traditional outpatient services offer.
Individual and Group Therapy: Therapy plays a critical role in drug and alcohol rehab. UMR rehab coverage often includes individual counseling, group therapy sessions, and family therapy, all of which are integral to the recovery process.
Medication-Assisted Treatment (MAT): For some, recovery involves medication to manage cravings or withdrawal symptoms. UMR may cover FDA-approved medications as part of a comprehensive treatment plan.
The Importance of Aftercare in Rehab
A significant aspect of rehabilitation is aftercare, which includes ongoing support to help prevent relapse after completing a treatment program. UMR may cover some aftercare services, such as:
Counseling and Therapy: Continuing therapy after rehab can be essential for maintaining sobriety. UMR plans often include coverage for outpatient therapy sessions that take place after the primary rehabilitation program.
Support Groups: Many individuals benefit from attending support groups such as Alcoholics Anonymous (AA) or Narcotics Anonymous (NA). While these groups are typically free, UMR may cover some of the counseling associated with these programs.
Relapse Prevention Programs: These programs offer strategies and skills to avoid falling back into addiction, which can be an essential part of long-term recovery.
Key Factors to Consider When Using UMR Insurance for Rehab
When evaluating UMR rehab coverage, consider the following factors to make the most of your benefits:
Deductibles and Co-Pays: Understanding how much you’ll need to pay upfront and what your co-payments will be for services is important for budgeting your rehab journey.
Out-of-Pocket Maximums: Every UMR plan has an out-of-pocket maximum, which is the most you’ll have to pay in a year before your insurance covers 100% of services. Reaching this limit during rehab can relieve you of additional financial burdens.
Limitations and Exclusions: Some UMR plans may have limitations on the length of treatment covered or exclusions for certain types of therapy or medication. Always verify these before starting a program.
Conclusion
UMR rehab coverage can offer significant financial relief for those seeking drug and alcohol rehabilitation in Arizona. By understanding your specific plan, choosing in-network facilities, and being aware of the services covered, you can navigate the process of addiction treatment with greater ease. If you are unsure of what your UMR plan includes, contacting UMR directly or speaking with a rehabilitation center's billing department can help you make informed decisions about your recovery.