Prior authorization (PA) is a process that requires healthcare providers to obtain approval from insurance companies before certain medications are dispensed to patients. While intended to ensure cost-effectiveness and appropriate medication use, the process can sometimes lead to delays in patient care.
The time required for prior authorization services based on multiple factors, including the insurance provider, type of medication, and the efficiency of communication between healthcare entities.
Factors Affecting Prior Authorization Timelines
Several factors influence how long the PA process takes:
Insurance Provider Policies – Different insurers have varying processing times and requirements.
Medication Type – Specialty drugs or high-cost medications may require additional review steps.
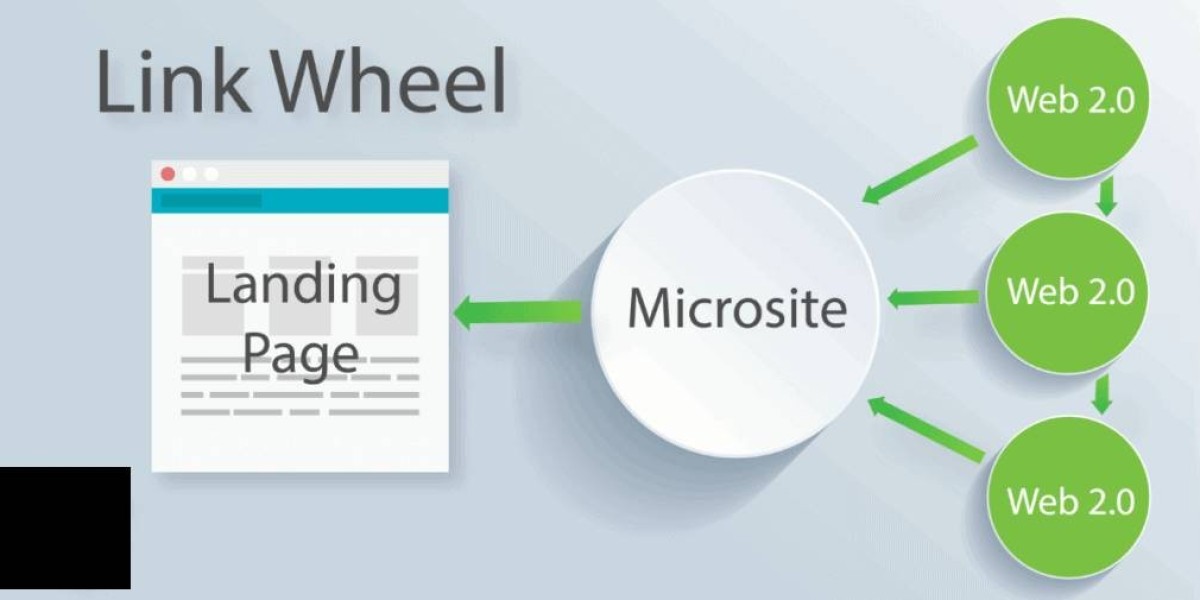
Electronic vs. Manual Submission – Electronic prior authorization (ePA) is generally faster than paper-based requests.
Healthcare Provider Responsiveness – Delays in submitting necessary documentation can prolong processing time.
Payer Backlogs – High volumes of requests may slow down approval times.
General Timeline for Prior Authorization
The time required for prior authorization can range from a few hours to several weeks. Typical timelines include:
Immediate to 24 hours – Some automated ePA systems process requests almost instantly.
1 to 3 Business Days – Many standard PA requests are reviewed and approved within this timeframe.
5 to 7 Business Days – Complex cases or those requiring additional documentation may take up to a week.
2 to 4 Weeks – If an initial request is denied and an appeal is necessary, the process can extend significantly.
Strategies to Expedite Prior Authorization
Providers and patients can take several steps to minimize delays:
Use Electronic Prior Authorization – Many insurers offer ePA systems that significantly reduce processing time.
Submit Complete Documentation – Providing all necessary clinical information upfront helps avoid rejections and resubmissions.
Follow Up with the Insurer – Regular communication with the insurance provider can keep the request moving forward.
Consider Alternative Medications – If delays persist, discussing covered alternatives with the provider can help.
Engage Patient Advocacy – Patients contacting insurers directly may sometimes expedite approvals.
Conclusion
The time required for prior authorization varies widely depending on multiple factors. While some approvals may be granted within hours, others may take weeks, especially if appeals are needed. By utilizing electronic submission, ensuring complete documentation, and proactively following up, both providers and patients can help expedite the process and ensure timely access to necessary medications.