The intersection of regulatory compliance and financial health has never been more critical for healthcare providers. With MIPS quality measures dictating Medicare reimbursements and operational inefficiencies draining revenue, practices face a dual challenge: delivering exceptional care while navigating complex reporting requirements.
This blog explores how medical billing consulting services empower providers to turn compliance into a competitive edge, ensuring both patient outcomes and profitability thrive in 2024.
The Evolution of MIPS Quality Measures in 2024
MIPS quality measures are the cornerstone of the Merit-Based Incentive Payment System (MIPS), which evaluates providers on four performance pillars:
Quality (50% of score): Patient outcomes, preventive care, and chronic disease management (e.g., “Breast Cancer Screening” or “Diabetes: Eye Exam”).
Cost (30%): Resource utilization efficiency, including surgical supplies and post-acute care expenses.
Improvement Activities (15%): Initiatives like mental health integration or community health programs.
Promoting Interoperability (25%): Seamless EHR data exchange and patient access to records.
In 2024, CMS introduced stricter benchmarks for MIPS quality measures, including:
New Telehealth Metrics: Tracking virtual care effectiveness for chronic conditions.
Health Equity Requirements: Reporting demographic data to address care disparities.
Patient-Reported Outcomes: Incorporating feedback on pain management or recovery experiences.
For example, a family practice must now report metrics like “Preventive Care and Screening: Tobacco Use” while ensuring EHR systems capture patient-reported data accurately.
Why Providers Struggle with MIPS Quality Measures
Despite their importance, many practices falter due to:
1. Data Fragmentation
Siloed EHR systems fail to consolidate data needed for MIPS quality measures, such as vaccination rates or post-op readmissions.
Nurses spend hours manually reconciling records from multiple platforms.
2. Coding Inconsistencies
Misusing CPT codes (e.g., 99213 vs. 99214 for office visits) skews Cost category scores.
Undercoding complex procedures (e.g., 47563 for laparoscopic cholecystectomy) leads to revenue leaks.
3. Regulatory Fatigue
Frequent CMS updates to MIPS quality measures overwhelm small practices. In 2024, 15 new measures were added, including those for behavioral health integration.
4. Financial Risks
A clinic with
2MinMedicarerevenueriskslosing
2MinMedicarerevenueriskslosing180K annually for poor MIPS performance.
How Medical Billing Consulting Services Drive Success
Medical billing consulting services bridge clinical and financial operations, ensuring alignment with MIPS quality measures while maximizing revenue. Key strategies include:
1. Holistic Workflow Audits
Consultants analyze workflows to identify gaps in MIPS quality measures reporting. For instance, a pediatric clinic improved its “Immunization Registry Reporting” score by 40% after consultants streamlined EHR data entry.
2. Advanced Coding Solutions
Experts audit claims for accuracy, ensuring codes like 12002 (wound repair) or 45380 (colonoscopy) reflect care complexity. This reduces denials by 30–50% and aligns with MIPS Cost benchmarks.
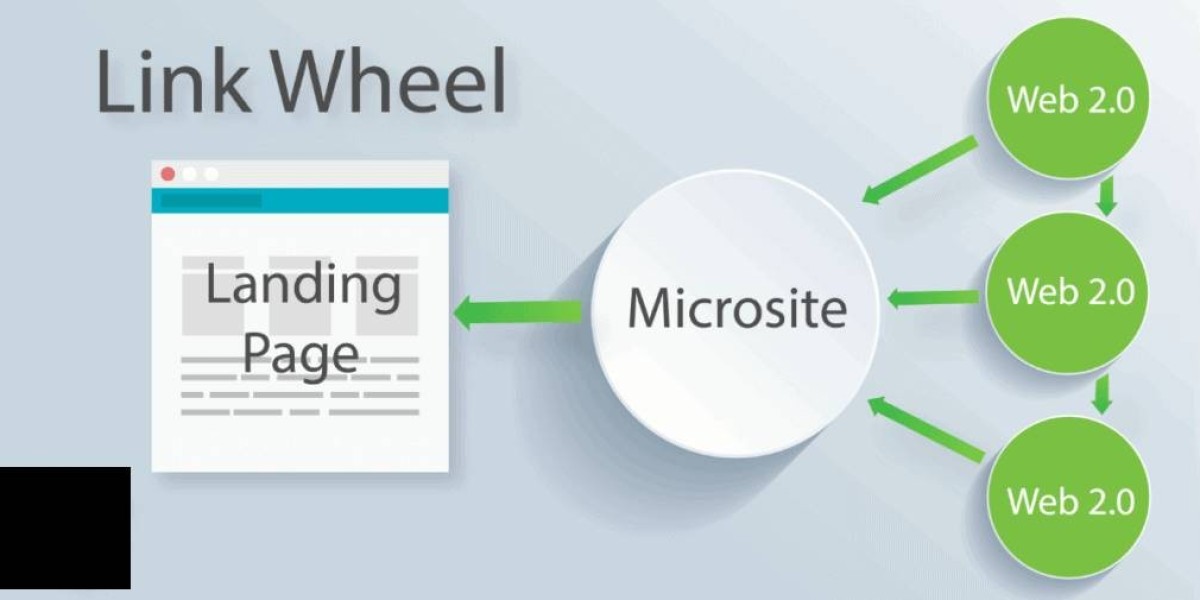
3. Technology-Driven Compliance
AI tools auto-populate MIPS quality measures fields in EHRs, reducing manual entry errors.
Predictive analytics flag high-risk patients (e.g., diabetics with uncontrolled HbA1c), enabling proactive interventions.
4. Staff Empowerment
Training programs teach clinicians to document patient interactions in ways that satisfy MIPS quality measures, such as recording smoking cessation counseling (measure #226).
Case Study: A Rural Clinic’s Turnaround
A rural primary care clinic faced:
A MIPS Quality score of 35/100 due to incomplete preventive care documentation.
28% claim denial rate from coding errors.
After partnering with medical billing consulting services:
Quality score jumped to 82/100 via optimized tracking of measures like “Statin Therapy for Cardiovascular Disease.”
Denials dropped to 8% after correcting CPT codes for chronic care management (99490).
The clinic earned $28K in MIPS incentives and reduced administrative costs by 25%.
Benefits of Integrating MIPS & Billing Expertise
Avoid Penalties: Proactively address gaps in MIPS quality measures reporting.
Boost Revenue: Resolve underpayments and denials with precision coding.
Enhance Patient Care: Align workflows with outcome-driven metrics.
Leverage Technology: Automate compliance and billing processes.
Future-Proof Operations: Stay ahead of CMS updates with expert guidance.
Why QPPMIPS Stands Out
QPPMIPS combines deep expertise in MIPS quality measures and medical billing consulting services to deliver:
Custom Compliance Plans: Tailored strategies for your specialty and size.
End-to-End Support: From claims scrubbing to MIPS submission.
Cutting-Edge Tools: AI-powered analytics and EHR integrations.
Transparent Reporting: Real-time dashboards for billing and compliance KPIs.
Conclusion: Elevate Your Practice in 2024
MIPS quality measures and medical billing consulting services are not just compliance checkboxes—they’re catalysts for growth. By optimizing reporting accuracy, reducing denials, and aligning care with CMS benchmarks, practices can secure reimbursements, avoid penalties, and reinvest in patient care.
Ready to optimize MIPS compliance and revenue?
Email: info@qppmips.com | Call: (888) 902-1035 | Visit: qppmips
Read more: Medical Billing & MIPS Reporting: Keys to 2024 Compliance