One of the most effective methods is by integrating insurance credentialing services and medical billing services into a unified system. While both services are essential on their own, combining them can significantly enhance your practice’s performance and profitability.
This article explores how integrated credentialing and billing processes work, the challenges of operating them separately, and the benefits healthcare providers gain from a unified approach.
1. Understanding the Basics: Insurance Credentialing and Medical Billing
Before diving into the benefits of integration, let’s first understand what these services entail.
1.1 What Are Insurance Credentialing Services?
Insurance credentialing is the process by which healthcare providers become authorized to offer services to patients covered by specific insurance companies. It includes:
Verifying a provider's qualifications, licenses, and experience
Ensuring compliance with payer and healthcare regulations
Ongoing maintenance, revalidation, and updates
⚠️ Note: Credentialing delays or errors can result in claim denials and revenue loss.
1.2 What Are Medical Billing Services?
Medical billing services is the process of submitting and following up on insurance claims for services rendered. It includes:
Coding procedures and diagnoses
Managing patient invoices
Handling claim denials and appeals
Ensuring accurate and timely reimbursement
⚠️ Note: Inefficiencies or errors in billing can cause underpayments, denials, or delayed payments—directly impacting your bottom line.
2. The Disconnect: Challenges of Separate Credentialing and Billing Systems
Many practices keep credentialing and billing as distinct functions. While manageable, this often leads to the following problems:
2.1 Delayed Revenue Cycle
Claims may be denied if the provider’s credentialing isn't updated in time.
Billing teams might unknowingly submit claims for uncredentialed providers.
2.2 Lack of Communication
Credentialing updates may not reach the billing team on time.
This can result in claims being filed with outdated or incorrect information.
2.3 Increased Risk of Denials
Delays in credentialing or incomplete registration may lead to rejections.
Resolution can take weeks, hurting cash flow.
2.4 Administrative Burden
Managing two separate vendors or systems increases costs.
It creates duplicated effort and hinders operational efficiency.
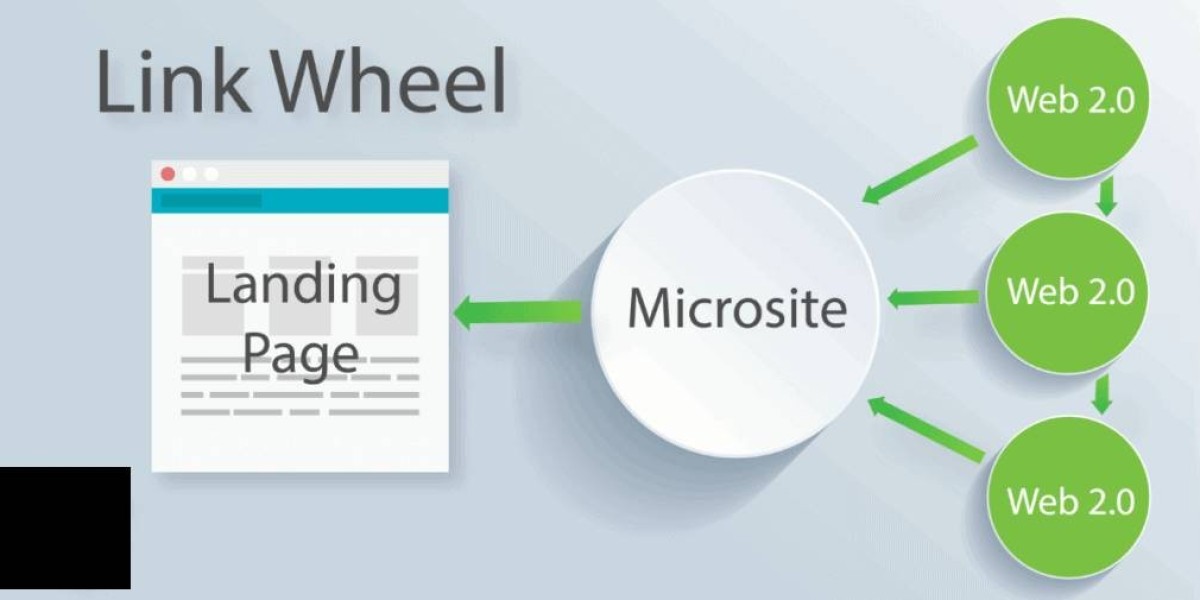
3. The Solution: Integrated Credentialing and Billing Services
Merging both services into a single streamlined process helps resolve these challenges. Here's how:
3.1 Seamless Communication Between Teams
Credentialing updates are instantly shared with billing staff.
Reduces risk of billing errors due to outdated provider data.
✅ Example: When a new physician is credentialed with a payer, billing begins cleanly from day one.
3.2 Faster Onboarding of New Providers
Simultaneous credentialing and billing setup reduce downtime.
Speeds up reimbursement and provider utilization.
3.3 Reduced Claim Denials and Rejections
Access to real-time credentialing data enables accurate billing.
Common credentialing errors like incorrect NPIs or missing effective dates are minimized.
3.4 Improved Revenue Cycle Management
Aligns all stages: payer validation, eligibility checks, claims, appeals.
Enables better tracking and optimization of the entire revenue cycle.
4. Financial Benefits of Integrated Services
Aside from workflow improvements, integration offers measurable financial gains:
4.1 Increased Collections
Accurate, first-time claim submissions mean quicker payments.
Fewer denials mean less rework and higher revenue capture.
4.2 Shorter Accounts Receivable (A/R) Cycles
Claims are submitted promptly post-credentialing.
Payments are received faster, improving cash flow.
4.3 Lower Administrative Costs
Single vendor/team reduces redundancy and staff training needs.
Easier management and greater scalability.
4.4 Better Financial Forecasting
Unified systems provide greater transparency into revenue trends.
Helps with planning, cash flow prediction, and growth initiatives.
5. Operational Benefits for Healthcare Practices
Integration also offers significant functional advantages:
5.1 Enhanced Compliance and Accuracy
Insurance credentialing services and medical billing services must comply with regulations.
Integrated teams catch inconsistencies and maintain adherence to payer rules.
5.2 Centralized Data and Reporting
Unified systems allow access to comprehensive practice data.
Better visibility into provider productivity, contract performance, and revenue metrics.
5.3 Greater Provider Satisfaction
Timely credentialing and billing reduce provider frustration.
Ensures they get paid quickly and can focus on patient care.
5.4 Streamlined Audits and Reviews
Organized documentation simplifies audits and insurance verifications.
Consistent records improve internal reviews.
6. Choosing the Right Partner for Integrated Services
Not all vendors are equally equipped. Look for a partner who provides:
✔️ Expertise in both credentialing and billing
✔️ Customized solutions based on your practice size and specialty
✔️ Advanced tools for automation, workflow, and reporting
✔️ Transparent communication with real-time updates
✔️ A strong history of lowering denials and boosting collections
? Avoid vendors who treat credentialing as a one-time task or lack alignment between the two services.
7. Case Study: The Impact of Integration
A mid-sized internal medicine practice faced frequent denials and cash flow issues due to separate credentialing and billing vendors. After switching to an integrated provider, they saw:
? 35% decrease in claim denial rate
? A/R days reduced from 52 to 30
? 20% increase in monthly revenue within six months
⚡ Provider onboarding time cut in half
This transformation was achieved by uniting credentialing and billing into a single, continuous workflow.
8. Final Thoughts
In today’s competitive healthcare environment, inefficiencies in the revenue cycle are costly. Integrating insurance credentialing and medical billing services provides a strategic advantage through:
✅ Faster reimbursements
✅ Fewer denials
✅ Stronger compliance
✅ Better provider and patient experiences
Forward-thinking practices are moving away from siloed systems and adopting integrated approaches—gaining operational harmony and a stronger bottom line.