In nursing, report writing is fundamental for ensuring the continuity and quality of patient care. Effective communication between healthcare professionals hinges on clear, concise, and accurate why reporting is important for nurses that document everything from patient conditions to treatments and care plans. Nursing reports serve not only as a way to hand off information during shift changes but also as an essential legal document that could be used in medical disputes.
Timely and well-written reports help in avoiding miscommunication, errors, and even harm to patients. Nurses must include all vital information, updates on patient progress, and any immediate needs or concerns. Additionally, report writing supports accountability and provides a comprehensive view of the patient’s care history, which is valuable for future reference and research.
Moreover, well-maintained reports are crucial for legal documentation. If ever a medical error or malpractice case arises, detailed reports are instrumental in providing a factual account of the care provided. Proper documentation can protect both the patient and healthcare providers by demonstrating that all required care was administered according to best practices.
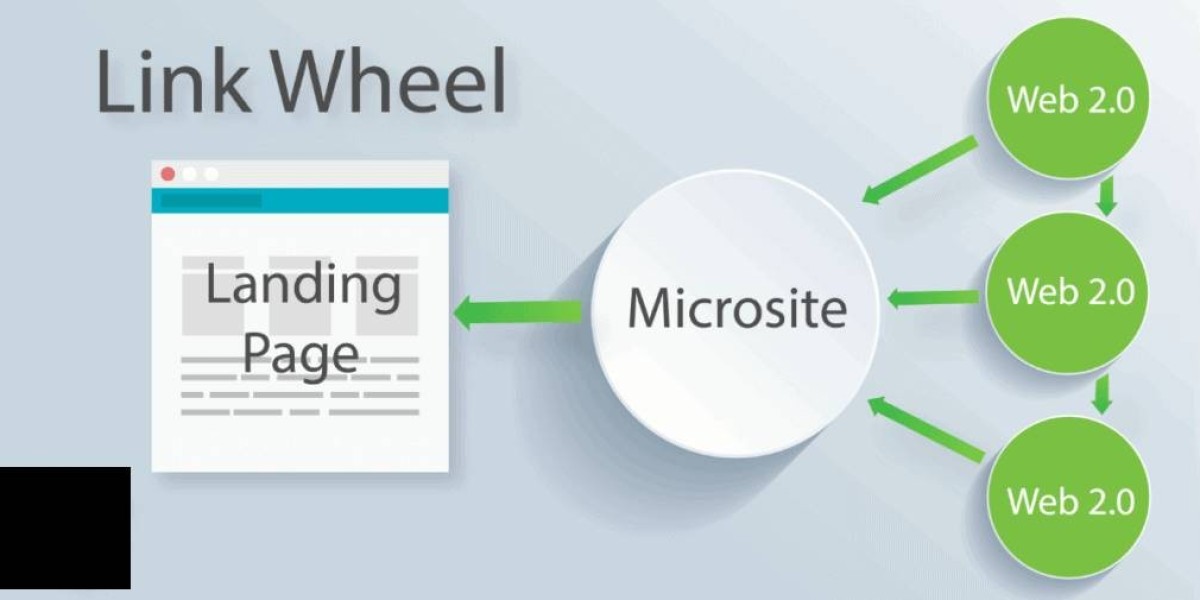
Another significant aspect of report writing is its contribution to inter-professional collaboration. Nurses often work in interdisciplinary teams, and clear reports ensure that every member of the team is up to date with the latest developments. This improves patient outcomes by aligning everyone’s efforts toward a shared goal of optimal care.
For nursing students and professionals looking to improve their report writing skills, resources such as templates, guidelines, and training modules can be highly beneficial. Practicing effective report writing will ensure nurses can communicate efficiently, mitigate risks, and uphold the standards of the nursing profession.