It can be like attempting to solve a complex puzzle while navigating the intricacies of neurology medical billing. Neurology offices frequently encounter major obstacles in attaining effective revenue cycles due to particular coding requirements, changing insurance regulations, and a high chance of denials.
However, what if there was a method to streamline the procedure while enhancing the financial results? The essential elements of neurology billing will be discussed in this article, along with typical mistakes, methods for improving accuracy, and how technology is transforming billing procedures.
1. Understanding the Basics of Neurology Medical Billing
Neurology billing is unique due to the specialized nature of neurological treatments, which often involve diagnostic tests, therapeutic procedures, and prolonged patient care.
- Key Billing Codes: Neurology billing requires mastery of CPT (Current Procedural Terminology) and ICD-10 codes, such as those for EEGs, EMGs, and complex neurological diagnoses.
- Modifier Usage: Proper application of modifiers ensures that services are billed appropriately and not rejected for lack of clarity.
2. Common Challenges in Neurology Medical Billing
Despite its importance, neurology billing is rife with challenges:
- Complex Documentation: Neurological procedures require detailed documentation to justify billing codes.
- Frequent Coding Updates: The medical billing landscape undergoes regular changes, increasing the risk of errors.
- High Denial Rates: Insufficient documentation, incorrect coding, or lack of pre-authorization often lead to claim denials.
3. Best Practices for Streamlining Neurology Billing
a. Ensure Accurate Coding and Documentation
- Invest in ongoing training for staff to stay updated on coding guidelines.
- Implement a documentation checklist to ensure all procedures and diagnoses are recorded correctly.
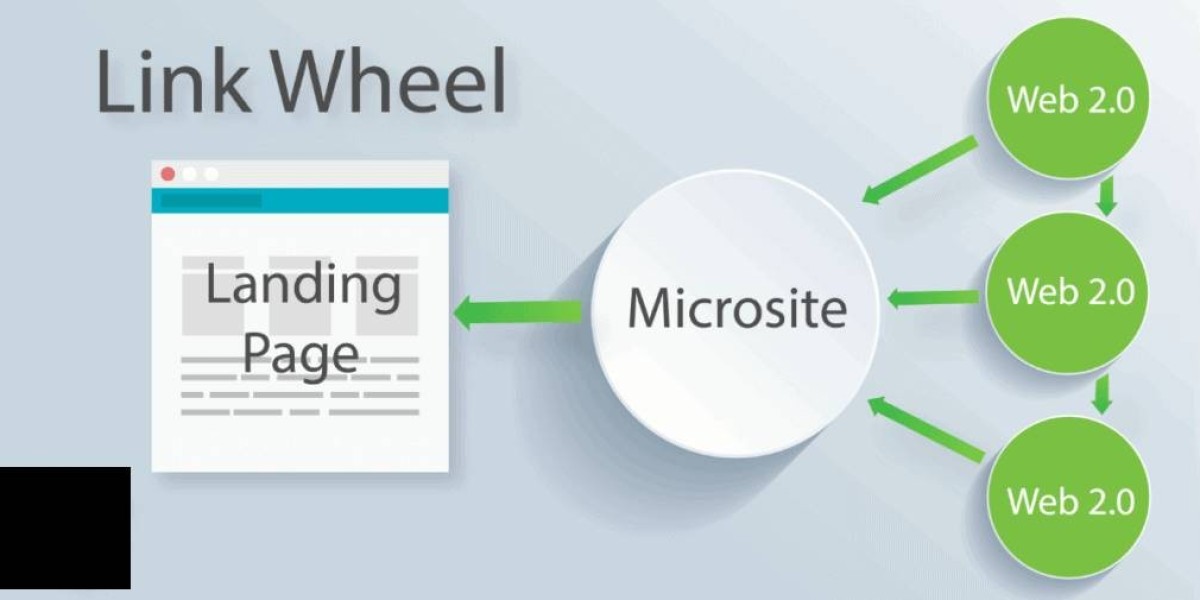
b. Leverage Technology for Efficiency
- Medical Billing Software: Tools like Kareo and AdvancedMD streamline billing workflows, reduce errors, and improve claim submission rates.
- AI-Powered Auditing: Artificial intelligence can analyze claims for potential errors before submission.
c. Focus on Pre-Authorization
Many neurology procedures require pre-authorization. Establish a robust system to verify insurance requirements and obtain approvals before scheduling procedures.
d. Partner with a Specialized Billing Service
Outsourcing to a neurology-specific billing service can significantly improve accuracy and efficiency while reducing the administrative burden on in-house staff.
4. Key Metrics to Track for Success
Monitoring performance is crucial for optimizing your billing process. Focus on these metrics:
- First-Pass Resolution Rate (FPRR): Measures the percentage of claims approved on the first submission.
- Days in Accounts Receivable (AR): Tracks the time it takes to receive payment after a claim is submitted.
- Denial Rate: Identifies the percentage of claims denied and highlights areas needing improvement.
5. Up-to-Date Statistics Supporting Neurology Billing Efficiency
- According to the American Medical Association, 9% of all medical claims are denied, with neurology among the most affected specialties.
- Practices using advanced billing software report a 25% reduction in claim denials and a 20% increase in revenue within the first year.
Conclusion
Mastering neurology medical billing requires a proactive approach, combining accurate documentation, robust technology, and regular staff training. By addressing common challenges and implementing best practices, neurology practices can improve revenue, reduce denials, and enhance operational efficiency.