T
umor models serve as invaluable tools, bridging the gap between laboratory research and clinical applications. They replicate various aspects of tumor growth, progression, and therapy responses, allowing scientists to explore cancer biology in a controlled environment.
This article examines the significance, types, applications, and future directions of tumor models in oncology research.
What Are Tumor Models?
Tumor models are experimental systems designed to mimic the development, behavior, and treatment response of tumors. These models are used to investigate tumor biology, test new therapies, and explore mechanisms of drug resistance. By simulating the tumor microenvironment, they provide insights into interactions between cancer cells, the immune system, and surrounding tissues.
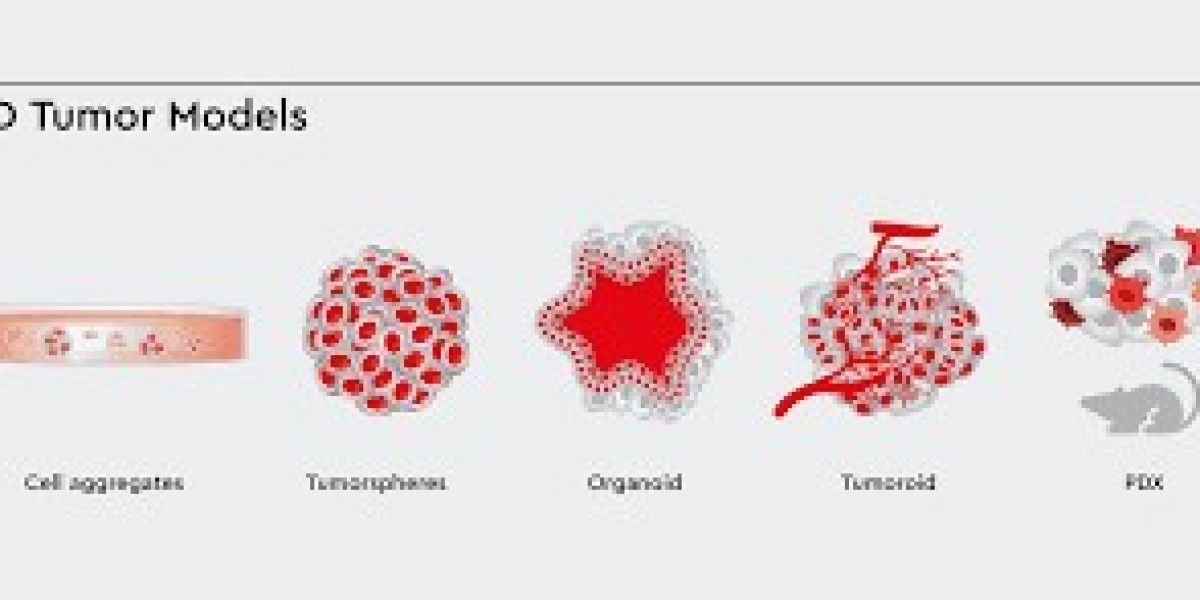
Types of Tumor Models
1. In Vitro Models
- 2D Cell Cultures:
Tumor cells are grown on flat surfaces in a monolayer.- Advantages: Cost-effective, simple to set up, and useful for high-throughput screening.
- Limitations: Lack of three-dimensional architecture limits their ability to replicate the complexity of tumors.
- 3D Cell Cultures:
Spheroids and organoids provide a three-dimensional structure that better mimics in vivo tumor growth and interactions.- Advantages: Closer representation of tumor microenvironments and treatment responses.
- Limitations: Limited ability to simulate systemic effects like metastasis.
2. In Vivo Models
These involve studying tumors in living organisms, typically animals, to capture systemic interactions.
Syngeneic Models:
Tumor cells from the same species are implanted into immunocompetent animals, preserving immune system interactions.- Applications: Immunotherapy and drug testing.
- Limitations: Do not use human cells, reducing translational relevance.
Patient-Derived Xenograft (PDX) Models:
Human tumor tissues are transplanted into immunocompromised animals, maintaining the original tumor’s genetic and histological properties.- Applications: Personalized medicine and drug screening.
- Limitations: Immunocompromised hosts limit immune-response studies.
Genetically Engineered Mouse Models (GEMMs):
Mice are genetically modified to develop tumors spontaneously.- Applications: Cancer initiation, progression, and metastasis studies.
- Limitations: High cost and time-intensive development.
Orthotopic Models:
Tumor cells are implanted into the organ of origin (e.g., pancreatic cancer cells into the pancreas), replicating the native microenvironment.- Applications: Metastasis and organ-specific cancer studies.
- Limitations: Require advanced imaging techniques for monitoring.
Carcinogen-Induced Models:
Tumors are induced using carcinogens like chemicals or radiation.- Applications: Studying environmental causes of cancer and tumor evolution.
- Limitations: Long development times and limited reproducibility.
Humanized Mouse Models:
Mice engrafted with human immune cells or tissues, enabling studies of human tumor-immune interactions.- Applications: Immunotherapy research, such as CAR-T cell therapy.
- Limitations: Expensive and challenging to develop.
Applications of Tumor Models
Understanding Tumor Biology
Tumor models help unravel mechanisms of tumor initiation, growth, invasion, and metastasis. They also enable studies of the tumor microenvironment, including interactions with immune and stromal cells.Drug Development and Testing
- Evaluate the efficacy, toxicity, and resistance mechanisms of potential cancer therapies.
- Test drug combinations to optimize treatment regimens.
Immunotherapy Research
- Syngeneic and humanized mouse models are critical for studying immune responses to cancer and developing immunotherapies like immune checkpoint inhibitors and CAR-T cells.
Metastasis Studies
- Orthotopic and GEMMs allow researchers to study how tumors spread to distant organs and test anti-metastatic therapies.
Personalized Medicine
- PDX models enable the testing of treatments on patient-specific tumors, offering a pathway to tailored cancer therapies.
Challenges and Limitations
Human vs. Animal Models
- Species differences can lead to discrepancies in tumor behavior and treatment responses, limiting the translational relevance of animal studies.
Complexity of Human Tumors
- Many models fail to replicate the heterogeneity and microenvironment of human cancers fully.
Ethical Concerns
- The use of animals in research raises ethical issues, driving the search for alternatives like organoids and computational models.
Cost and Time
- Advanced models, such as GEMMs and humanized mice, require significant financial and time resources.
Immunocompromised Hosts
- Models like PDXs, which rely on immunocompromised animals, cannot study immune-related therapies effectively.
Future Directions
Organoids and Organs-on-a-Chip
- Advanced in vitro systems that replicate human tissues are becoming increasingly sophisticated, offering alternatives to animal models.
CRISPR-Cas9 Technology
- Gene-editing tools are streamlining the creation of genetically engineered models, reducing development times.
Artificial Intelligence
- AI is being used to analyze data from tumor models, predict drug responses, and optimize experimental designs.
Combination Models
- Hybrid approaches, such as humanized PDXs, combine the strengths of multiple models for more comprehensive studies.
Ethical Alternatives
- Efforts to reduce reliance on animal models include developing advanced in vitro systems, computational simulations, and machine-learning tools.
Conclusion
The Tumor models are essential for understanding cancer biology, developing therapies, and advancing personalized medicine. While no single model perfectly replicates human cancer, the combination of in vitro, in vivo, and hybrid systems provides a robust framework for translational research.
With advancements in technology and ethical considerations, tumor models will continue to play a critical role in combating cancer, bringing us closer to improved outcomes and innovative treatments for patients worldwide.