Introduction to Automated Revenue Cycle Management in USA
The healthcare industry in the USA is evolving rapidly, and so are the technologies that support it. One of the most transformative advancements is Automated Revenue Cycle Management in USA. This approach leverages cutting-edge technology to streamline the entire revenue cycle, from patient registration to final payment collection. Automated RCM reduces errors, speeds up processes, and ultimately improves the financial health of healthcare providers. If you're looking to boost efficiency and revenue, automation is the game-changer you need.
What is Automated Revenue Cycle Management?
Definition and Key Concepts
Automated Revenue Cycle Management refers to the use of software tools and artificial intelligence (AI) to manage the administrative and clinical functions involved in billing and revenue collection. This automation covers tasks like eligibility verification, medical coding, claims submission, and payment posting.
Difference Between Manual and Automated RCM
While traditional manual RCM depends heavily on human input, automated RCM uses technology to handle repetitive tasks. This drastically reduces human error, accelerates workflows, and allows staff to focus on complex issues that require personal attention.
The Importance of Automation in Healthcare Revenue Cycles
Healthcare providers face numerous challenges in managing revenue cycles, including increasing claim denials, complex payer rules, and patient billing confusion. Automation offers a scalable solution to these problems, helping providers keep pace with growing patient volumes and regulatory demands.
Benefits of Automated Revenue Cycle Management in USA
Increased Accuracy
Automated systems minimize coding mistakes and data entry errors, ensuring claims are clean and accepted by payers more often.
Faster Claims Processing
By automating claim scrubbing and submission, payments come faster, improving the provider’s cash flow.
Reduced Denials and Rejections
AI-powered systems identify potential claim issues before submission, lowering denial rates significantly.
Improved Cash Flow
Faster payments and reduced denials mean steady cash flow for healthcare organizations.
Enhanced Compliance
Automation helps maintain HIPAA and payer compliance through built-in checks and secure data handling.
Key Features of Automated Revenue Cycle Management Systems
AI-Powered Coding and Billing
Machine learning algorithms assist with accurate medical coding, reducing errors and speeding up billing.
Eligibility Verification Automation
Instantly confirms patient insurance coverage before service delivery, preventing claim denials.
Automated Claims Scrubbing
Claims are reviewed for errors automatically, ensuring they meet payer requirements before submission.
Real-Time Analytics and Reporting
Dashboards provide up-to-date financial insights, enabling smarter decision-making.
Patient Payment Portals
Facilitate easy online bill payments and payment plan management for patients.
Challenges Addressed by Automated RCM
Manual processes are prone to errors, delays, and compliance issues. Automation tackles these by providing consistent, accurate, and fast workflows that adapt to payer changes and patient needs seamlessly.
How Automated RCM Transforms Healthcare Providers’ Operations
With automated revenue cycle management, healthcare providers experience:
- Streamlined workflows reducing administrative burden
- Higher patient satisfaction through transparent billing
- More predictable revenue streams and fewer write-offs
Why Choose a Provider Specialized in Automated Revenue Cycle Management in USA
Specialized providers understand the unique needs of healthcare facilities and bring the right mix of technology and expertise to deliver results tailored to your practice.
Spotlight on MyBillingProvider.com for Automated RCM Services
Customized Automated Solutions
MyBillingProvider.com offers tailored automated revenue cycle management services designed specifically for healthcare providers in the USA.
Seamless Integration and Support
Their solutions integrate with existing EHR systems, providing continuous support and updates to keep your operations smooth.
Proven Results
Clients have experienced improved collections, fewer denials, and enhanced operational efficiency.
Impact of Automated RCM on Patient Experience
Automation enables clear, timely billing communication, making it easier for patients to understand their financial responsibilities and pay promptly, which boosts satisfaction and loyalty.
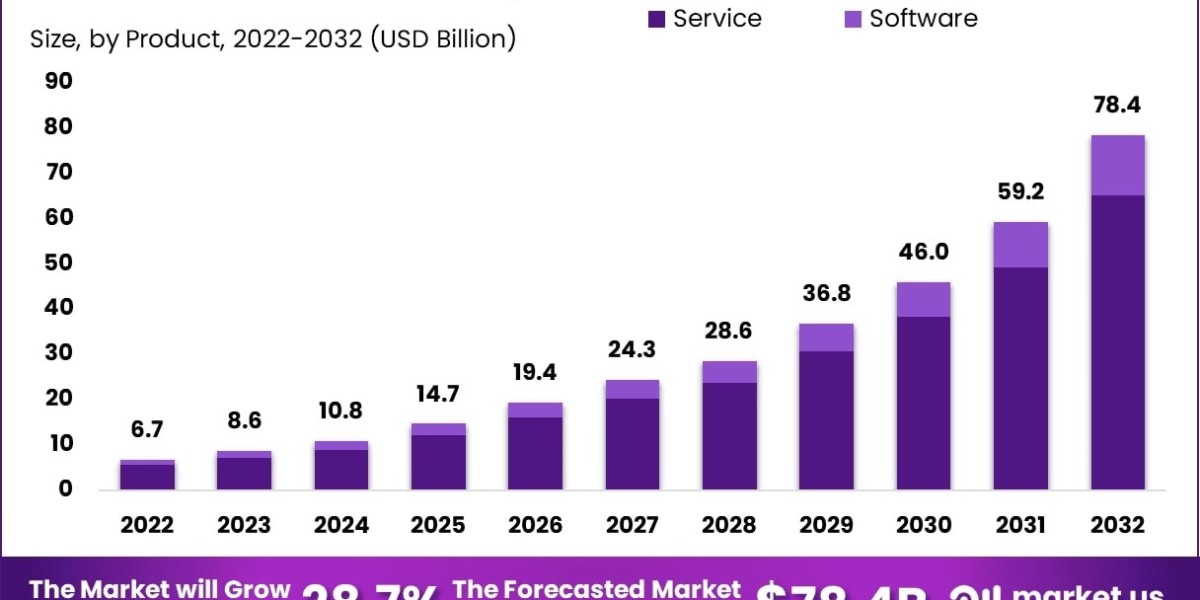
Future Trends in Automated Revenue Cycle Management
The future will see greater AI sophistication, blockchain-based security, and personalized patient financial engagement tools becoming standard in automated RCM.
Tips for Implementing Automated RCM Successfully
- Choose a provider with healthcare expertise
- Ensure your existing systems are compatible
- Train staff to work alongside automated tools
- Monitor KPIs to track improvements and identify issues
Conclusion
Automated Revenue Cycle Management in USA is revolutionizing how healthcare providers manage billing and payments. By embracing automation, providers reduce errors, accelerate payments, and enhance compliance—all while improving patient satisfaction. Companies like MyBillingProvider.com are at the forefront of this transformation, offering scalable, efficient solutions tailored to healthcare needs. If you want to future-proof your revenue cycle and maximize financial performance, automated RCM is the way to go.