Introduction
Accounts Receivable (AR) recovery is a critical component of revenue cycle management in the healthcare industry. It refers to the process of collecting outstanding payments from insurance companies and patients. A high AR balance can indicate inefficiencies in claim processing, leading to financial instability for healthcare providers.
Hospitals, clinics, and medical practices face numerous challenges in managing AR, including claim denials, delayed reimbursements, and underpayments. Without a proper AR recovery strategy, healthcare providers may experience revenue losses, impacting their ability to deliver quality patient care. By implementing efficient AR recovery solutions, healthcare organizations can optimize cash flow, minimize bad debt, and improve overall financial performance.
Understanding AR Recovery in Healthcare
AR recovery involves tracking, managing, and collecting overdue payments from insurance providers and patients. The process requires identifying reasons for payment delays and taking appropriate action to recover lost revenue. Some of the most common causes of high AR balances include:
Claim denials due to coding errors or missing documentation
Delayed payments from insurance companies
Patient payment delays or outstanding balances
Underpayments resulting from incorrect claim processing
A structured approach to AR recovery helps healthcare providers address these challenges efficiently. It involves consistent follow-ups, resubmission of denied claims, and proactive engagement with payers to resolve disputes.
Key Steps in AR Recovery
1. Identifying Unpaid and Denied Claims
The first step in AR recovery is analyzing all outstanding claims and categorizing them based on the reason for delay or denial. This includes:
Reviewing Explanation of Benefits (EOBs) and remittance advice from insurance companies.
Identifying claims that require corrections or additional documentation.
Prioritizing high-value claims to recover maximum revenue quickly.
2. Claim Resubmission and Follow-Ups
Once errors are identified, denied claims must be corrected and resubmitted within the allowable time frame. Consistent follow-ups with insurance companies help track claim status and ensure timely reimbursements.
3. Insurance Appeals Management
If claims are denied due to technical or administrative issues, healthcare providers can file appeals. A strong appeals process involves:
Understanding insurance policies and reasons for denials.
Submitting supporting documentation and medical records.
Communicating with payers to negotiate fair settlements.
4. Patient Collections and Payment Plans
Patients also contribute to outstanding AR balances. Hospitals must establish clear billing policies, offer flexible payment plans, and educate patients on their financial responsibilities. Sending timely reminders and offering multiple payment options can improve patient collections.
5. AR Aging Analysis and Reporting
Tracking AR aging reports helps identify long-overdue accounts. AR reports categorize outstanding payments based on the number of days overdue (30, 60, 90, or 120+ days). Addressing older accounts promptly prevents revenue loss.
Benefits of Effective AR Recovery
A well-managed AR recovery process provides several benefits to healthcare providers:
1. Improved Cash Flow
Timely collection of outstanding payments ensures a steady cash flow, helping healthcare facilities cover operational expenses and invest in better patient care.
2. Reduced Claim Denials and Write-Offs
By addressing claim errors proactively and filing appeals when necessary, healthcare providers can minimize denials and reduce revenue write-offs.
3. Enhanced Compliance with Billing Regulations
Proper AR management ensures compliance with payer policies, reducing the risk of financial penalties and audits.
4. Increased Operational Efficiency
With a structured AR recovery strategy, healthcare providers can focus on patient care rather than administrative burdens.
Best Practices for AR Recovery
1. Automate Billing and Claim Tracking
Using advanced billing software helps streamline claim submissions, track payments, and identify potential issues before they escalate.
2. Implement a Denial Prevention Strategy
Preventing denials is more cost-effective than recovering lost revenue. Healthcare providers should:
Ensure accurate coding and documentation.
Verify patient insurance details before service.
Train staff on common billing errors and how to avoid them.
3. Monitor AR Aging Reports Regularly
Analyzing AR aging reports helps providers track overdue payments and take immediate action on older accounts.
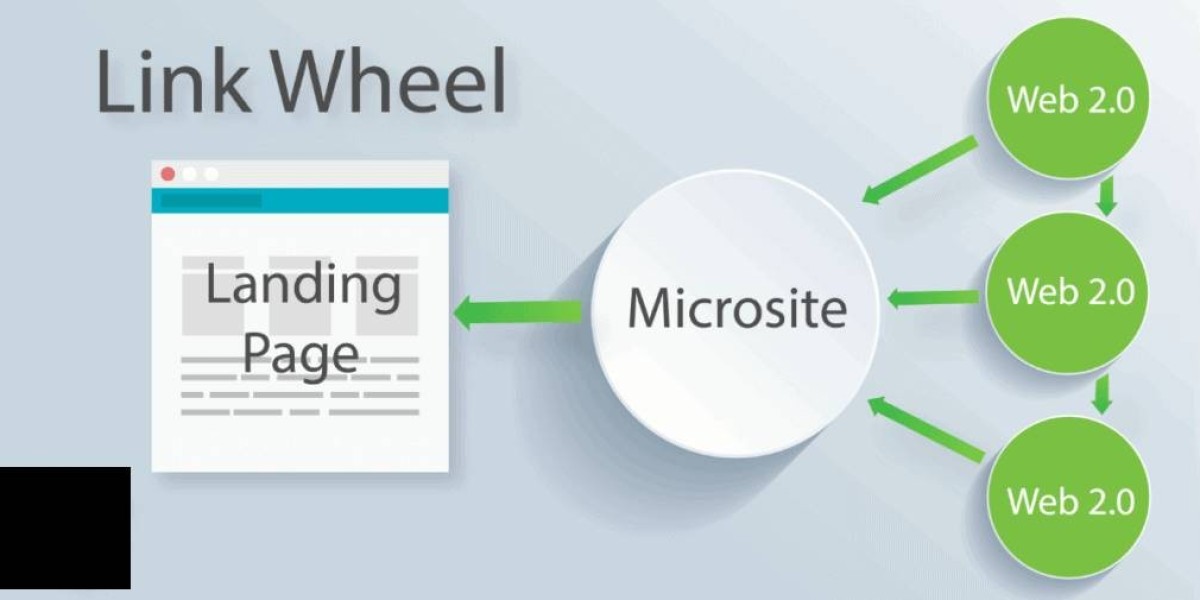
4. Partner with a Professional AR Recovery Service
Outsourcing AR recovery to a professional medical billing company can improve collection rates and reduce administrative stress.
Why Choose Medbillingrcm for AR Recovery Services?
Medbillingrcm is a trusted provider of AR recovery solutions, helping healthcare organizations recover outstanding revenue efficiently. Our team of billing experts specializes in:
✔ Insurance verification and eligibility checks
✔ Claim resubmission and follow-ups
✔ Denial management and appeals processing
✔ Patient collections and payment plan solutions
✔ Detailed financial reporting and AR analytics
Conclusion
AR recovery is essential for healthcare providers to maintain financial stability and improve cash flow. Delayed reimbursements and outstanding claims can significantly impact hospital revenue. By implementing an effective AR recovery strategy, hospitals can reduce claim denials, speed up payments, and ensure compliance with industry regulations. Partnering with a professional AR recovery service like Medbillingrcm can help healthcare providers recover lost revenue efficiently and focus on delivering quality patient care.