The Future of Healthcare: Transforming Patient Outcomes Through Data Integration
In today’s rapidly evolving healthcare landscape, data plays a crucial role in driving better patient outcomes, improving operational efficiencies, and enabling more informed decision-making. As healthcare organizations increasingly rely on vast amounts of digital information—from patient records and diagnostic images to research data and real-time monitoring—the need for seamless communication among disparate systems has never been more apparent. In this digital age, the concept of integrating health data isn’t just a technological challenge, but a critical factor in improving the quality, safety, and efficiency of patient care. Health Information Interoperability -Optimizing Data Sharing Across Stakeholders for Faster Decision-Making
Understanding Health Information Interoperability
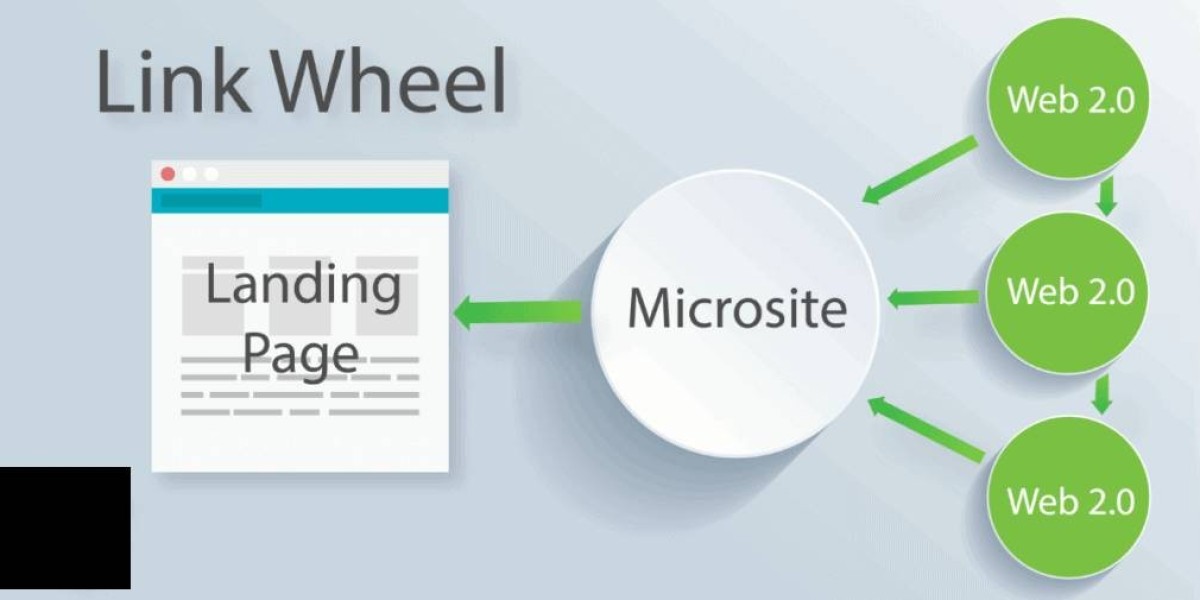
At its core, health information interoperability refers to the ability of different information systems, devices, and applications to access, exchange, integrate, and cooperatively use data in a coordinated manner. It is not simply about connecting various systems; it’s about ensuring that the data shared is meaningful, secure, and available in real time for the clinicians and administrators who need it. With modern healthcare increasingly driven by data analytics, predictive modeling, and precision medicine, achieving robust interoperability is paramount for delivering timely, efficient, and personalized patient care.
Interoperability extends beyond just technical connectivity. It involves aligning standards, policies, and workflows to ensure that data exchanged between providers, payers, patients, and even public health agencies is accurate and actionable. As systems become more interconnected, the opportunities to identify health trends, predict epidemics, and reduce inefficiencies across the healthcare continuum increase dramatically.
The Driving Forces Behind Data Integration
Several factors are driving the need for improved health information interoperability:
Patient-Centered Care: Patients today are more informed and proactive about their health. They expect their healthcare providers to have immediate access to their comprehensive medical history, regardless of where they received previous care. Interoperable systems ensure that a patient’s information follows them, allowing for seamless transitions between primary care, specialists, and emergency services.
Regulatory Requirements: Governments and regulatory bodies around the world are pushing for higher standards in data sharing to reduce medical errors, enhance public health responses, and promote transparency. Policies such as the Health Information Technology for Economic and Clinical Health (HITECH) Act in the United States have incentivized the adoption of electronic health records (EHRs) and the exchange of health information.
Technological Advancements: The rapid development of cloud computing, big data analytics, and artificial intelligence is transforming how health information is collected and used. These technologies enable real-time data processing and decision support, which can be critical in emergency care and chronic disease management.
Cost Reduction and Efficiency: Healthcare systems are continually under pressure to reduce costs while maintaining or improving the quality of care. Efficient data sharing minimizes redundant tests, streamlines administrative processes, and enhances overall operational efficiency, directly impacting the bottom line.
Challenges in Achieving Interoperability
Despite the clear benefits, several challenges remain on the path to full-scale interoperability:
Data Silos: One of the most significant barriers is the existence of data silos, where information is isolated within a single organization or system. These silos prevent the smooth flow of data and can lead to fragmented care.
Variability in Standards: While many standards exist for health data exchange (such as HL7, FHIR, and DICOM), not all systems adhere to them uniformly. This variability can create compatibility issues when different healthcare entities attempt to share information.
Privacy and Security Concerns: Health data is highly sensitive, and breaches can have severe consequences for both patients and organizations. Ensuring that data is securely transmitted and stored while maintaining compliance with regulations like HIPAA is a complex but essential aspect of interoperability.
Cost and Resource Constraints: Implementing interoperable systems often requires significant upfront investment in technology and training. Smaller practices and rural hospitals may struggle to allocate the necessary resources, widening the digital divide in healthcare.
Strategies for Optimizing Data Sharing
To overcome these challenges and harness the full potential of health information interoperability, stakeholders can adopt several strategies:
Adoption of Universal Standards: Encouraging the use of universal data exchange standards such as Fast Healthcare Interoperability Resources (FHIR) can simplify the process of sharing data between disparate systems. Standardization not only enhances compatibility but also accelerates the integration process across the industry.
Collaborative Ecosystems: Fostering collaboration among healthcare providers, technology vendors, government agencies, and patients is critical. By working together, stakeholders can develop common goals, share best practices, and create integrated systems that serve the entire healthcare ecosystem.
Investing in Secure Technologies: Enhancing cybersecurity measures is non-negotiable. Advanced encryption methods, multi-factor authentication, and robust data governance frameworks are essential to protect sensitive health information while allowing for its seamless exchange.
Leveraging Cloud Computing: Cloud-based platforms offer scalable and cost-effective solutions for data storage and sharing. They enable real-time access to patient data and support the implementation of innovative tools like machine learning algorithms that can predict patient outcomes and optimize treatment plans.
Policy and Incentive Alignment: Governments and regulatory bodies can play a pivotal role by aligning policies and incentives that encourage the adoption of interoperable systems. Financial incentives, technical support, and clear regulatory guidelines can help overcome resource constraints, particularly in underfunded institutions.
Real-World Impacts of Interoperability
The benefits of achieving health information interoperability are already being witnessed in various settings:
Emergency Response: In emergency scenarios, the ability to access a patient’s comprehensive medical history can be lifesaving. When emergency departments have immediate access to information about allergies, medications, and previous conditions, they can make faster, more informed decisions that reduce the risk of adverse events.
Chronic Disease Management: For patients with chronic conditions such as diabetes or heart disease, continuous monitoring and regular updates to their care plans are crucial. Interoperable systems facilitate the seamless sharing of data between primary care providers, specialists, and home health devices, ensuring that treatment plans are up-to-date and effective.
Research and Public Health: Researchers benefit from interoperability by having access to large, diverse datasets that can be used to study disease patterns, treatment outcomes, and the effectiveness of new therapies. Public health agencies, in turn, can use this data to monitor and respond to outbreaks, allocate resources more effectively, and implement preventive measures.
Patient Engagement: When patients have secure access to their health records, they become active participants in their care. Patient portals and mobile apps that integrate with EHRs empower individuals to track their health metrics, schedule appointments, and communicate with their healthcare teams more efficiently.
The Future of Health Information Interoperability
Looking ahead, the future of healthcare is deeply intertwined with the continued evolution of health information interoperability. Emerging technologies such as blockchain offer the potential to enhance data security and traceability, ensuring that every piece of information is verified and tamper-proof. Additionally, the integration of artificial intelligence and machine learning into health data systems promises to unlock new insights, from personalized treatment plans to predictive analytics that can preemptively address potential health crises.
The move toward a more connected, data-driven healthcare environment also means that interoperability will become a foundational element of global health strategies. International collaborations, such as those seen in pandemic responses, highlight the need for standardized data exchange protocols that transcend national borders. As healthcare systems worldwide continue to digitize and interconnect, the role of interoperability in driving innovation, reducing costs, and improving patient care will only grow more prominent.
Conclusion
The journey toward achieving full-scale health information interoperability is complex, yet the potential rewards are immense. By breaking down data silos, aligning standards, and investing in secure, scalable technologies, the healthcare industry can pave the way for a future where information flows seamlessly across every level of care. This transformation will not only enhance the efficiency and quality of healthcare delivery but also empower patients to take charge of their own health in ways previously unimaginable. As we continue to innovate and collaborate, the promise of a fully interconnected healthcare ecosystem moves ever closer to reality, fundamentally reshaping how we diagnose, treat, and manage health conditions for generations to come.