Medical billing is an essential component of physician revenue cycle management, ensuring that healthcare providers are properly reimbursed for their services. However, billing errors are common in medical practices, leading to claim denials, delayed payments, compliance risks, and financial losses. Even minor mistakes can have a significant impact on cash flow and operational efficiency.
To help healthcare providers improve billing accuracy, this blog will cover common billing errors physicians make and provide practical solutions to avoid them.
Understanding Physician Billing and Revenue Cycle Management
Medical billing involves the process of:
✅ Submitting claims to insurance payers (Medicare, Medicaid, private insurers)
✅ Ensuring proper coding using CPT, ICD-10, and HCPCS codes
✅ Managing claim denials and following up on outstanding payments
✅ Handling patient billing and collections
Errors in any of these areas can lead to:
- Revenue loss due to denied or rejected claims
- Compliance violations and penalties
- Administrative inefficiencies that slow down cash flow
By implementing strong physician revenue cycle management strategies, providers can reduce billing mistakes, speed up reimbursements, and maintain financial stability.
Common Billing Errors Physicians Make and How to Avoid Them
1. Inaccurate Patient Information
One of the most frequent billing errors is incorrect patient details, such as:
- Misspelled names
- Wrong date of birth
- Incorrect insurance policy numbers
- Outdated insurance coverage
Even small errors can cause claim denials and payment delays.
Solution:
✅ Verify patient information at every visit using real-time eligibility checks.
✅ Train front-desk staff to double-check insurance details.
✅ Use automated patient registration systems to minimize human errors.
2. Missing or Incorrect Medical Codes
Medical billing relies on accurate coding using ICD-10, CPT, and HCPCS codes. Errors such as:
- Incorrect diagnosis codes
- Mismatched procedure codes
- Omitting necessary modifiers
- Upcoding (billing for a higher service level than provided)
- Undercoding (failing to report services performed)
can result in claim denials, audits, and compliance penalties.
Solution:
✅ Train coders and physicians in accurate medical coding.
✅ Use billing software with built-in code validation.
✅ Conduct regular coding audits to identify and correct mistakes.
3. Not Verifying Insurance Eligibility and Coverage
Many claims are denied because providers fail to check insurance eligibility before rendering services. Patients may have:
- Inactive policies
- Out-of-network coverage
- Exceeded benefit limits
Solution:
✅ Use electronic eligibility verification tools before scheduling appointments.
✅ Confirm pre-authorizations for services that require approval.
✅ Educate front-desk staff on payer-specific coverage rules.
4. Missing Prior Authorizations
Certain procedures and treatments require prior authorization from insurers. Failure to obtain authorization can result in claim denials and lost revenue.
Solution:
✅ Maintain a database of procedures requiring prior authorization.
✅ Assign a dedicated team to track and follow up on authorizations.
✅ Use automated prior authorization tools to streamline approvals.
5. Failure to Document Medical Necessity
Payers require clear documentation proving that a service was medically necessary. Missing or vague documentation can lead to claim denials.
Solution:
✅ Ensure physicians document detailed patient notes supporting the diagnosis and treatment plan.
✅ Train staff on payer-specific documentation requirements.
✅ Conduct periodic documentation audits to improve compliance.
6. Duplicate Billing
Duplicate billing occurs when the same service is billed twice, often due to:
- Manual entry errors
- Lack of communication between billing staff
- Technical glitches in billing software
Duplicate claims lead to denials, compliance risks, and audits.
Solution:
✅ Use billing software that flags duplicate claims before submission.
✅ Establish internal checks to review claims before sending them to payers.
✅ Train staff to cross-check previous billing records.
7. Incorrect Use of Modifiers
Modifiers are essential for providing additional details about a service or procedure. Incorrect or missing modifiers can lead to claim rejections or underpayments.
Solution:
✅ Train coding staff on modifier rules for different payers.
✅ Use automated claim scrubbing tools to catch modifier errors.
✅ Refer to CMS and insurance guidelines for correct modifier usage.
8. Delayed Claim Submission
Each insurer has strict deadlines for claim submission. Late filing can result in:
- Claim denials with no appeal option
- Lost revenue due to missed deadlines
Solution:
✅ Implement automated billing workflows to ensure timely claim submission.
✅ Track payer-specific deadlines and set reminders.
✅ Conduct weekly reviews of pending claims to avoid delays.
9. Ignoring Claim Denials and Failing to Appeal
Many practices do not follow up on denied claims, leading to unnecessary revenue loss. Common reasons for denials include:
- Missing information
- Incorrect coding
- Lack of medical necessity
Solution:
✅ Set up a dedicated denial management team.
✅ Track denial trends and fix recurring issues.
✅ Appeal every denied claim where possible, providing additional documentation as needed.
10. Lack of Patient Payment Collection Strategies
Patient responsibility for medical bills is increasing. Failing to collect co-pays, deductibles, or outstanding balances can create financial strain for practices.
Solution:
✅ Implement clear payment policies and discuss costs upfront with patients.
✅ Offer multiple payment options (online portals, payment plans, credit card processing).
✅ Send timely billing reminders via email and text.
Best Practices for Reducing Billing Errors
To improve physician revenue cycle management, follow these best practices:
1. Invest in Billing and RCM Technology
✅ Use AI-powered billing software for claim accuracy.
✅ Automate eligibility verification and prior authorizations.
✅ Implement real-time claim tracking to prevent delays.
2. Regular Staff Training and Education
✅ Train coders and billers on ICD-10, CPT, and HCPCS updates.
✅ Conduct annual compliance training to prevent legal risks.
✅ Offer ongoing education on payer policy changes.
3. Perform Internal Billing Audits
✅ Review claims for accuracy before submission.
✅ Identify denial trends and root causes.
✅ Conduct monthly coding audits to reduce errors.
4. Strengthen Communication Between Departments
✅ Ensure front-desk staff, physicians, and billers collaborate.
✅ Establish standard workflows for documentation and coding.
✅ Hold regular team meetings to address billing challenges.
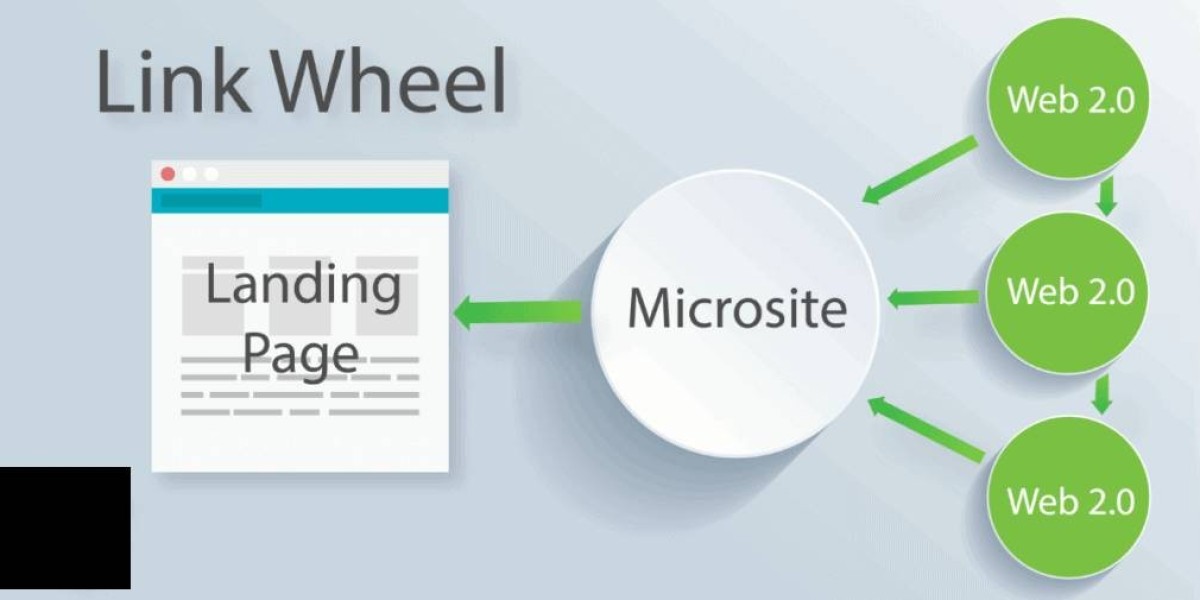
5. Outsource Billing to Experts
✅ Consider partnering with RCM service providers for efficiency.
✅ Outsourcing can reduce administrative burden and improve collections.
Conclusion
Billing errors are a major obstacle in physician revenue cycle management, leading to claim denials, compliance risks, and revenue loss. However, by implementing proactive strategies such as staff training, automated billing technology, denial management, and internal audits, healthcare providers can minimize mistakes and maximize reimbursements.
By focusing on accuracy, compliance, and efficiency, physicians can streamline their billing process, improve cash flow, and ensure financial success.