Nurse practitioners play a key role in modern healthcare by working alongside physicians to improve patient outcomes. This collaboration is essential in hospitals, clinics, and primary care settings, where both professionals contribute their expertise to deliver comprehensive medical care. A family nurse practitioner near me provides essential services while maintaining a partnership with doctors to address patient needs efficiently. The relationship between these healthcare providers is built on communication, shared responsibilities, and a commitment to delivering high-quality care.
Co-Management of Patient Treatment Plans
One of the most critical aspects of collaboration is the joint management of patient care. Nurse practitioners assess symptoms, perform physical exams, and diagnose conditions, while physicians provide oversight and specialized medical expertise when needed. This model of care allows patients to receive well-rounded treatment that integrates different perspectives.
In many cases, nurse practitioners handle routine care for chronic conditions like diabetes, hypertension, and asthma. They monitor patient progress, adjust medications, and educate individuals on lifestyle modifications. When complex cases arise, physicians step in to review and refine treatment plans. This dynamic partnership ensures patients receive appropriate care at every stage of their medical journey.
In emergency or acute care situations, co-management becomes even more vital. A physician may focus on advanced diagnostics and procedural interventions, while a nurse practitioner manages patient stabilization and follow-up care. This division of labor allows for efficient use of medical resources while maintaining high standards of treatment.
Shared Decision-Making Processes
Collaboration between nurse practitioners and physicians is rooted in shared decision-making. Both professionals bring their clinical knowledge and patient interactions to discussions on treatment options. When reviewing diagnostic results, medication plans, or surgical interventions, their combined expertise helps determine the best course of action.
Patients benefit significantly from this approach because it fosters well-informed treatment plans tailored to their needs. By incorporating the perspectives of both nurse practitioners and physicians, healthcare providers can ensure decisions align with medical best practices while also considering patient preferences.
When a treatment plan needs adjustment, nurse practitioners often take the lead in communicating changes to patients and ensuring they understand their next steps. Physicians provide additional insight when a case requires specialized knowledge. This seamless exchange of information contributes to a more effective healthcare system that prioritizes patient well-being.
Effective Communication Strategies
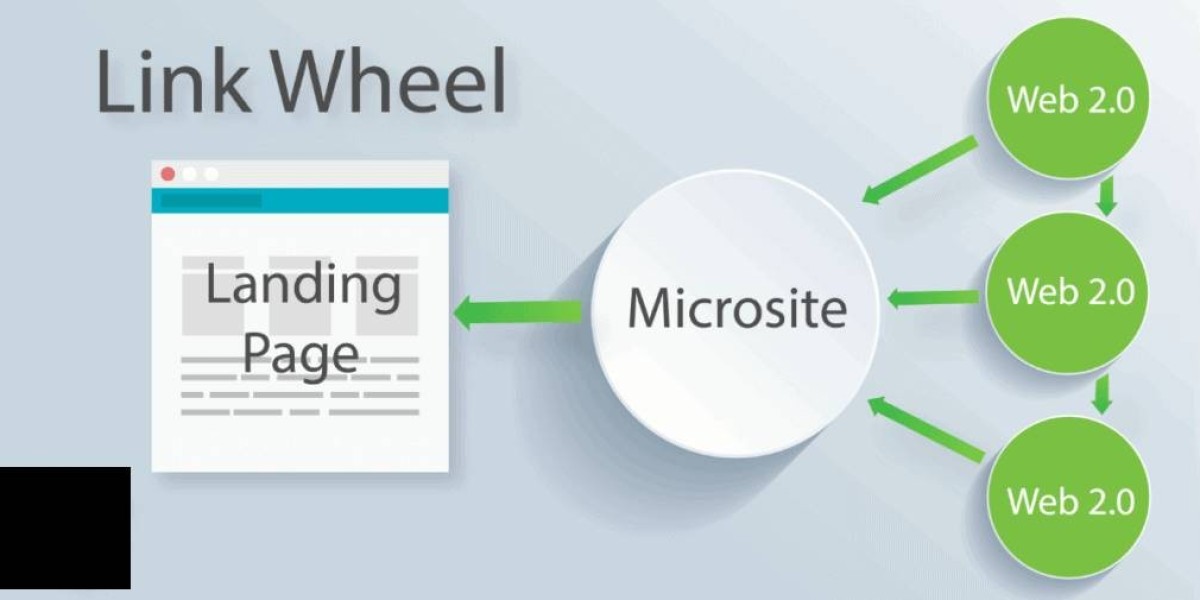
Strong communication is at the core of successful collaboration in clinical settings. Nurse practitioners and physicians must maintain clear and consistent dialogue to prevent medical errors and enhance patient safety. Regular meetings, electronic health records, and standardized reporting methods contribute to efficient information sharing.
One method used in many healthcare facilities is the use of interdisciplinary team meetings. These meetings allow nurse practitioners, physicians, and other healthcare professionals to discuss patient cases, review treatment progress, and address any concerns. Open communication in these settings fosters a supportive work environment where both roles complement each other.
Digital tools also play a key role in maintaining seamless communication. Electronic health records provide real-time updates on patient conditions, allowing both nurse practitioners and physicians to stay informed. Secure messaging systems enable quick consultations between providers, ensuring that urgent concerns receive immediate attention.
Delegation of Responsibilities and Tasks
A well-structured delegation of duties enhances efficiency in clinical environments. Nurse practitioners manage a wide range of tasks that allow physicians to focus on complex cases requiring specialized expertise. While physicians oversee medical procedures, nurse practitioners handle patient education, follow-ups, and preventive care.
In primary care settings, nurse practitioners conduct routine check-ups, administer vaccines, and manage medication refills. Their ability to handle these responsibilities independently reduces the workload on physicians and enhances access to healthcare services. In hospital settings, nurse practitioners may assist with post-operative care, monitor recovery progress, and coordinate discharge planning.
The delegation of tasks also strengthens patient-provider relationships. Since nurse practitioners spend more time interacting with patients, they provide valuable insights into a patient’s health status. Their close monitoring allows for early detection of potential complications, which can then be addressed in collaboration with physicians.
Joint Participation in Quality Improvement Initiatives
Beyond direct patient care, nurse practitioners and physicians work together on initiatives aimed at improving healthcare delivery. These efforts may involve refining clinical protocols, enhancing patient education strategies, or developing programs to address community health concerns.
Quality improvement initiatives often focus on reducing hospital readmissions, minimizing medical errors, and enhancing patient satisfaction. Nurse practitioners contribute by collecting patient feedback, tracking treatment outcomes, and implementing new care models. Physicians provide input on medical advancements and policy changes that impact healthcare practices.
In some cases, nurse practitioners and physicians collaborate on research projects that explore innovative treatment methods or evaluate existing healthcare policies. Their combined efforts lead to the development of evidence-based practices that improve patient care on a larger scale.
Fostering Interprofessional Relationships
Strong working relationships between nurse practitioners and physicians create a supportive clinical environment where healthcare providers can thrive. Mutual respect and recognition of each other’s expertise are key factors in building successful collaborations.
Many healthcare facilities implement mentorship programs where experienced physicians guide nurse practitioners in expanding their clinical skills. These programs provide opportunities for professional growth and strengthen the partnership between both roles.
Interprofessional collaboration also extends to working with nurses, pharmacists, therapists, and other healthcare providers. When all members of the medical team function cohesively, patients receive coordinated care that addresses their physical, emotional, and psychological needs.
Conclusion
The collaboration between nurse practitioners and physicians is a fundamental component of modern healthcare. Their combined efforts in co-managing treatment plans, engaging in shared decision-making, and maintaining effective communication result in improved patient outcomes. Delegating responsibilities, participating in quality improvement initiatives, and fostering strong interprofessional relationships contribute to a more efficient healthcare system. A family nurse practitioner near me plays an essential role in delivering accessible and comprehensive medical care by working closely with physicians to meet patient needs.