In the complex ecosystem of healthcare, delivering quality care is only one part of the equation. For healthcare practices to remain financially sustainable, they must ensure efficient and accurate reimbursement for the services they provide. This is where Medical Revenue Cycle Management becomes essential.
Medical RCM encompasses all the administrative and clinical functions that contribute to capturing, managing, and collecting revenue from patient services. This article provides a comprehensive look at medical revenue cycle management—its components, challenges, benefits, technologies, and how it directly impacts a provider’s financial performance.
What is Medical Revenue Cycle Management?
Medical Revenue Cycle Management refers to the systematic process that healthcare providers use to track patient care events from the initial appointment scheduling to the final payment of the balance due. It involves everything from verifying patient insurance to billing, coding, claims submission, denial management, and collections.
The primary goal of medical RCM is to maximize revenue generation, reduce administrative costs, and improve cash flow while maintaining compliance with healthcare regulations.
Key Stages of the Medical Revenue Cycle
Pre-Registration and Eligibility Verification
Collecting patient demographics, insurance details, and verifying coverage
Ensuring services are authorized and covered by the insurance provider
Patient Registration
Updating or confirming patient records at the time of the appointment
Capturing co-pay information and financial responsibility details
Medical Coding and Charge Capture
Translating clinical documentation into standardized codes (ICD-10, CPT)
Assigning accurate charges based on services rendered
Claim Submission
Preparing and submitting claims to insurance companies
Ensuring clean claims that reduce denial risks
Payment Posting
Applying received payments to patient accounts
Reconciling Explanation of Benefits (EOB) with billed charges
Denial Management
Reviewing, correcting, and resubmitting denied claims
Identifying root causes of denials and applying preventative measures
Patient Billing and Collections
Sending bills to patients for remaining balances
Offering support, payment plans, and follow-up for collections
Reporting and Analytics
Monitoring performance through KPIs such as A/R days, denial rates, and collection rates
Using data to improve workflow and financial outcomes
Why Medical Revenue Cycle Management is Important
Healthcare providers face increasing pressure from insurance companies, government regulations, and patients with high-deductible health plans. Without effective RCM, providers risk:
Delayed or lost reimbursements
High denial rates and write-offs
Compliance issues and potential audits
Poor patient financial experience
Revenue leakage
Effective medical RCM ensures that healthcare organizations are compensated quickly, accurately, and fully for the care they deliver.
Benefits of an Effective Medical RCM System
Faster Reimbursements
Clean claims and automated processes reduce turnaround times.Reduced Denials and Rejections
Accurate documentation, coding, and claim submission lowers the chances of denial.Improved Cash Flow
Consistent revenue inflow supports business continuity and growth.Better Patient Satisfaction
Clear billing and payment options enhance the patient experience.Regulatory Compliance
Helps maintain compliance with HIPAA, CMS, and payer-specific guidelines.Operational Efficiency
Reduces manual effort, administrative overhead, and billing cycle delays.
Challenges in Medical Revenue Cycle Management
Despite its benefits, medical RCM comes with several challenges:
Complex Coding Requirements: ICD-10, CPT, and HCPCS updates demand continuous training and accuracy.
Frequent Regulatory Changes: Policies from Medicare, Medicaid, and private payers often change.
High Denial Rates: Even minor data entry errors can cause delays and revenue loss.
Patient Payment Responsibility: With more patients on high-deductible plans, collecting balances becomes more difficult.
Disparate Systems: Lack of integration between EHR, billing, and practice management software can create inefficiencies.
The Role of Technology in Medical RCM
Modern RCM is driven by digital transformation. The use of technology in managing the revenue cycle has significantly improved speed, accuracy, and transparency.
Key Technologies in Medical RCM:
Electronic Health Records (EHR): Centralize patient data for seamless coding and billing
Medical Billing Software: Automates claim creation, submission, and tracking
Computer-Assisted Coding (CAC): Uses AI to recommend accurate codes based on documentation
Patient Portals: Allow patients to view bills, make payments, and communicate with billing staff
Analytics and Dashboards: Offer insights into revenue trends, denials, and performance metrics
Robotic Process Automation (RPA): Automates repetitive tasks such as eligibility checks and claim status follow-up
These tools reduce manual intervention, minimize errors, and improve claim resolution rates.
Outsourcing Medical Revenue Cycle Management
Many providers, especially small and mid-sized practices, choose to outsource RCM to specialized third-party vendors. These companies offer:
Experienced billing and coding teams
Up-to-date knowledge of payer requirements
Scalable services
Access to the latest billing technologies
Detailed reporting and insights
Benefits of Outsourcing:
Reduces administrative burden
Lowers staffing and technology costs
Improves collections and cash flow
Allows focus on patient care instead of billing tasks
However, providers must ensure that the RCM partner follows best practices for data security, transparency, and communication.
Key Performance Indicators (KPIs) in Medical RCM
To measure the effectiveness of medical revenue cycle management, healthcare providers monitor the following KPIs:
Days in Accounts Receivable (A/R)
Clean Claim Rate
First Pass Resolution Rate (FPRR)
Net Collection Rate
Denial Rate
Patient Collection Percentage
Bad Debt Write-Offs
Tracking these metrics helps identify bottlenecks and opportunities for improvement.
Best Practices for Medical Revenue Cycle Management
Verify Insurance Early:
Conduct eligibility checks and authorization before the patient visit.Accurate and Complete Documentation:
Providers must document services clearly to support correct coding.Ongoing Staff Training:
Keep billing and coding staff updated on regulation and payer changes.Automate Where Possible:
Use software and AI tools to streamline repetitive tasks and reduce manual errors.Regular Audits:
Conduct routine internal and external audits to ensure compliance and identify issues.Patient Engagement:
Educate patients about their benefits, bills, and payment options to improve collections.
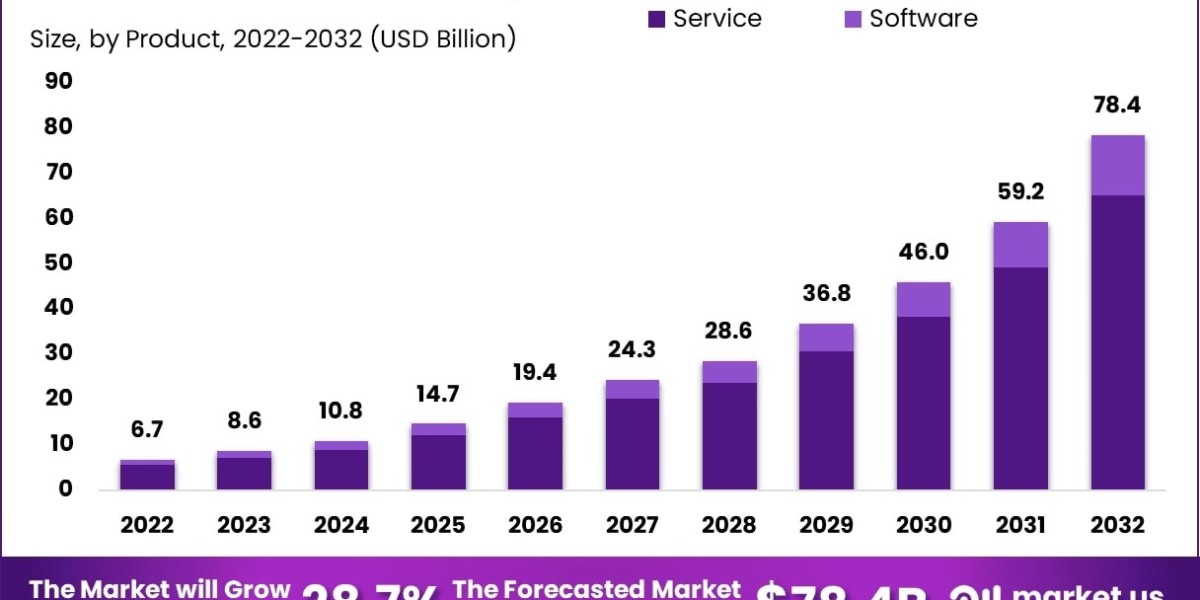
The Future of Medical Revenue Cycle Management
As the healthcare industry moves toward value-based care, the future of RCM will focus more on outcomes than volume. Key trends shaping the future include:
AI and Predictive Analytics: For identifying denial risks, coding errors, and collection challenges
Integrated RCM Platforms: Cloud-based systems that connect scheduling, billing, and EHR
Mobile Payment Solutions: Easy and flexible ways for patients to pay their bills
Personalized Financial Communication: Tailored payment plans and billing communication based on patient behavior
Blockchain for Secure Billing: Ensuring transparency and trust in claim transactions
Adopting these innovations will enable providers to remain competitive and financially healthy in a patient-first, data-driven world.
Conclusion
Medical Revenue Cycle Management is the heartbeat of financial performance in any healthcare setting. It ensures that care delivered translates into sustainable revenue while maintaining compliance and a positive patient experience.
By leveraging technology, outsourcing to experts when needed, and consistently optimizing each step of the cycle, providers can improve profitability, reduce denials, and enhance operational efficiency. In a rapidly changing industry, effective RCM is not just a process—it’s a strategic advantage.